Message from Program Director
Welcome to the Obstetrics and Gynecology Residency Program at Westchester Medical Center, the flagship of the Westchester Medical Center Health Network (WMCHealth). Our highly competitive academic program is unique in that it involves faculty and residents providing clinical care at both Westchester Medical Center and New York City Health and Hospitals/Metropolitan. The program seeks to provide residents with comprehensive clinical experience in Obstetrics and Gynecology in urban, suburban, and rural settings.
We provide extensive clinical experiences in general obstetrics and gynecology as well as subspecialty services such a gynecologic oncology, urogynecology, maternal fetal medicine, minimally invasive gynecologic surgery and pelvic pain, family planning, and reproductive endocrinology and infertility. It is our mission that a large component of the residents’ clinical training is focused on the care of under-represented minorities and high-risk populations. We are the first hospital system in the area to establish the Center for Women’s Health Equity. Our residents are actively involved in providing care for patients within the center and participate in the fundamental components of this program including educational curricula, research, and advocacy.
Our faculty are diverse, experienced, and deeply committed, with experience and training from all major academic centers in the country. The faculty and residents have worked hard to create a culture of psychological safety and inquiry within the residency program. Using state of the art technology for clinical care and education has helped us continue to keep up with advances in medical education and training. Faculty work closely with residents in research mentorship and career guidance, building professional relationships that last well beyond the four years of residency. Multiple members of our faculty have completed the APGO Surgical Education Scholars Program, and we continue to provide faculty development opportunities to continue to educate our faculty to be physician educators. Additionally, we have faculty who are ABOG board examiners and faculty who are nationally recognized for their research, including NIH funded faculty.
We have regular didactic sessions throughout the week on all services as well as a half day per week of protected didactic time for resident education. The residency didactic schedule includes didactic lectures, journal clubs, colposcopy conference, research meetings, CREOG reviews, and clinical leadership curriculum. There are monthly simulation sessions with the residents to learn gynecologic surgery, obstetric maneuvers, and safety procedures.
Westchester Medical Center is one of the Regional Perinatal Centers for New York State. Pregnant patients are transferred to Labor and Delivery from 10 affiliate hospitals, covering a seven-county region. In addition, Westchester Medical Center’s Institute for Women’s Health and Wellness is devoted to providing comprehensive women’s health to women throughout the Hudson Valley for which Westchester Medical Center is the flagship hospital. We care for some of the highest acuity in obstetrics and gynecology, complemented by lower risk complexity to provide the best overall exposure to our residents.
In summary, we offer unique and comprehensive clinical experience both within New York City and in Westchester County. Our residents graduate as incredible physicians and have found careers in General OB/GYN practices or have continued into fellowship training, many in leadership positions.
Thank you for your interest in our program. Please take some time to explore our website to learn more about what our program has to offer.
Sincerely,
Julia G. Keltz, MD, FACOG
Residency Program Director
Clinical Assistant Professor

Residency Leadership Team
 |
 |
 |
Angelica Sze, MD
Associate Program Director |
Sharifa Menon, MD
Assistant Program Director - Wellness |
Jessica Berrios-Elliott, MIS, C-TAGME
Program Manager |
Program's Mission
The department is committed in its goal of educating residents for their future role as specialists offering comprehensive care to all women and to enable them to achieve their professional goals of clinical practice, academia, or fellowship. Our residents provide care to patients throughout the Hudson Valley and New York City area, serving urban, suburban, and rural patient populations. The department believes that the rich diversity of its residents, faculty, and patient populations are key to its mission of educating outstanding health care professionals for the multicultural world.
Clinical Sites
Westchester Medical Center: Graduate Medical Education
Metropolitan: NYC Health + Hospitals/Metropolitan
Academic Partnership
New York Medical College

Ryan Residency Training Program
The OB-GYN Residency Program at Westchester Medical Center is part of the Kenneth J.Ryan Residency Training Program. The Ryan Program is a national initiative that supports OB-GYN residency programs to create training opportunities in abortion and contraception.
Center for Women's Health Equity
The Center for Women's Health Equity is the first program of its kind based in New York State’s Hudson Valley region, and has an initial aim of reducing the leading causes of death among pregnant women by integrating specialists in maternal-fetal medicine, whose expertise is the care of complex medical problems affecting pregnant women, with its heart and vascular program clinicians to take a more proactive and holistic view of elevated risk factors among women, particularly those of color.

Regional Perinatal Center
The Regional Perinatal Center (RPC) at Westchester Medical Center (WMC) is one of 18 Regional Perinatal Centers in New York State (NYS). We are committed to working with the NYS Department of Health and our affiliate hospitals to accomplish the goal of improving the health of pregnant women and newborns we serve in the Lower Hudson Valley Region. We partner with our 10 affiliate hospitals covering a seven county region and totaling more than 40,000 births annually.
- RPC (Regional Perinatal Center): "Level IV" Neonatal Intensive Care Nursery
A hospital which provides perinatal clinical services that meet the standards for a level III clinical program but also includes highly specialized services (e.g. ECMO, cardiac surgery, in utero procedures etc.) that may not be available at Level III facilities. The RPC has additional responsibilities for teaching, research, and out-reach as well as database management for its network of hospitals. The RPC is required to formulate an infrastructure to enhance integration of perinatal health care services to accomplish these goals using the tool of a "Regional Perinatal Forum."
Social Media
Follow us on Instagram: @nymcobgyn
FREIDA™ AMA Residency & Fellowship Programs Database (ama-assn.org) Program ID 2203521199
Educational Program
The Obstetrics and Gynecology Residency Program at Westchester Medical Center offers a continuously evolving educational curriculum which is heavily influenced by the residents’ valuable input and follows the educational objectives and core competencies established by the Council on Resident Education in Obstetrics and Gynecology (CREOG).
During this 4-year program, our residents divide their time between Westchester Medical Center and Metropolitan Hospital, affording them an incredible breadth and depth of exposure to diverse patient populations, all subspecialties within OB/GYN (gynecologic oncology, maternal fetal medicine, urogynecology, minimally invasive gynecologic surgery, pediatric and adolescent gynecology, family planning, reproductive endocrinology and infertility) and essential exposure to primary care in women’s health.
In addition to the clinical experience, our residents have protected time for an extensive didactics program at both clinical sites. Each week the residents and attendings dedicate two half-days to teaching at Westchester Medical Center and Metropolitan Hospital, with activities including Grand Rounds, Resident Report, Resident Lecture Series, and Simulation training. Our simulation program includes low fidelity trainers as well as advanced technology trainers such as robotic simulation and high-fidelity surgical models. Supplementary to the formal didactics program are daily MFM teaching rounds, weekly perinatal-neonatal conference, biweekly perinatal conference, tumor board, pre-op conference, and CREOG preparation.
Our program is fully supportive of and compliant with the ACGME clinical and educational work hour regulations, and we understand the importance of resident wellness and wellbeing. Our goal is to provide a high-quality educational experience that emphasizes time for adequate rest and out-of-hospital activities. Therefore, all residents have four weeks of vacation, four additional personal days, and all participate in our established clinical leadership curriculum. We prioritize community partnership and volunteerism, and the residents participate in off campus community service projects and wellness programming.
Rotation Calendar
The following is a representation of the rotation schedules for each PG year.
PGY1 Rotations
|
Metropolitan Hospital
|
Westchester Medical Center
|
|
Obstetrics & Gynecology
|
Obstetrics
|
|
Subspecialty: REI, Family Planning, MFM
|
Gynecology Oncology
|
|
Continuity Clinic
|
Night Float
|
|
|
Benign Gyn, MIGS, Urogyn, REI
|
PGY2 Rotations
|
Metropolitan Hospital
|
Westchester Medical Center
|
|
Obstetrics & Gynecology
|
Obstetrics: Antepartum, MFM, Ultrasound
|
|
Subspecialty: MFM, Ultrasound, REI, Family planning
|
Benign Gyn, MIGS, Urogyn, REI
|
|
Continuity Clinic
|
Night Float
|
|
|
Family Planning |
PGY3 Rotations
|
Metropolitan Hospital
|
Westchester Medical Center
|
|
Continuity Clinic
|
Obstetrics
|
|
Night Float
|
Benign Gyn, MIGS, Urogyn, Family Planning - Chief
|
|
Ambulatory: Gyn Clinic, REI, Urogyn, MIGS, Family planning
|
|
Gynecology Oncology
|
PGY4 Rotations
|
Metropolitan Hospital
|
Westchester Medical Center
|
|
Obstetrics & Gynecology – Chief
|
Obstetrics – Chief
|
|
Continuity Clinic
|
Gynecology: Benign Gyn, MIGS, Urogyn - Chief
|
|
|
Gynecology Oncology - Chief
|
|
Night Float - Chief
|
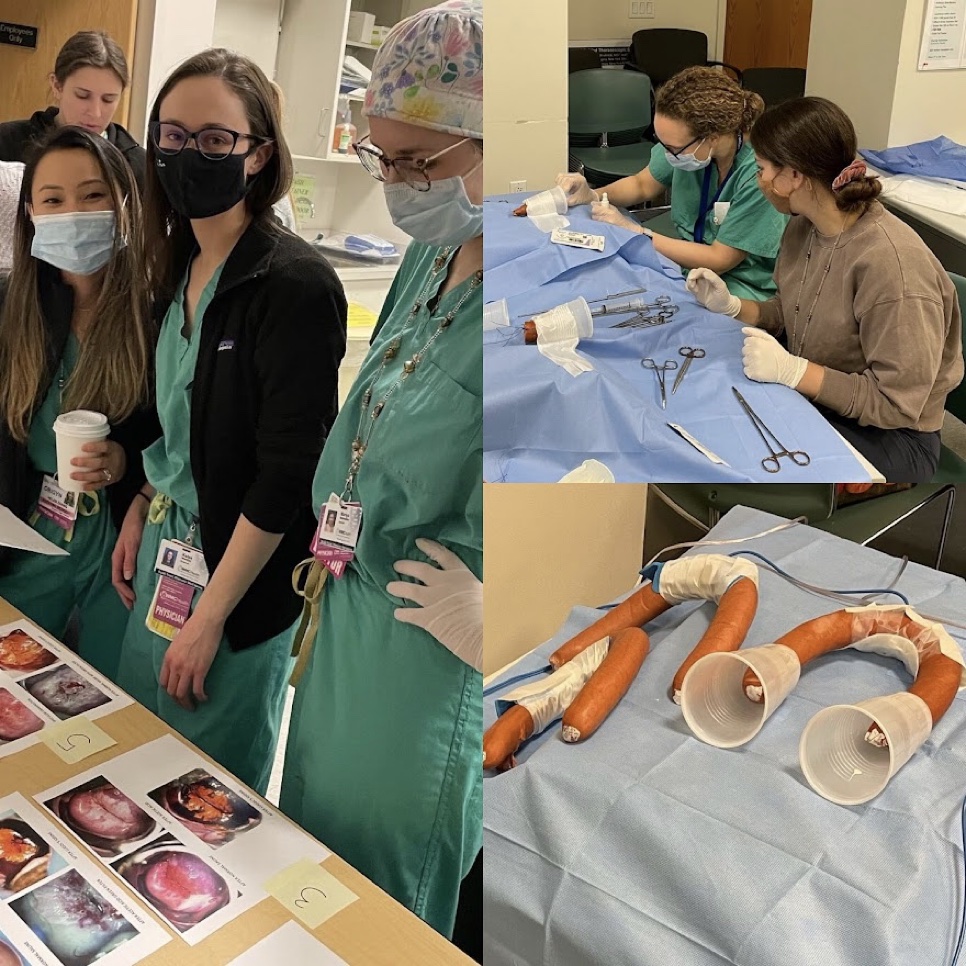
Simulation Training Program
Our Simulation program is a comprehensive, hands-on curriculum, aimed at teaching residents the fundamentals of Obstetrics and Gynecology. Our curriculum consists of a four-year rotating schedule of simulation sessions throughout the academic year including both Obstetric simulations and Gynecologic simulations. Our program is constantly evolving to ensure that residents have access to a curriculum that will allow them to grow and improve as physicians.
The American Board of Obstetrics and Gynecology (ABOG) now requires that all residents graduating after May 31, 2020 must pass the Fundamentals of Laparoscopic Surgery (FLS) exam. The simulation curriculum includes preparing residents for the surgical skills component of this examination.

Post-Match Intern Preparation Curriculum
Before the start of residency, our incoming interns participate in two curricula aimed to prepare the incoming interns for residency on day 1.
Readiness for Residency Curriculum: 4 sessions (3 zoom and 1 in person) to help prepare incoming interns for the new challenges of residency.
Topics included in this curriculum are:
- Resilience & Gratitude
- Time Management & Priorities
- Evolving Your Learning Skills
- Mission & Values
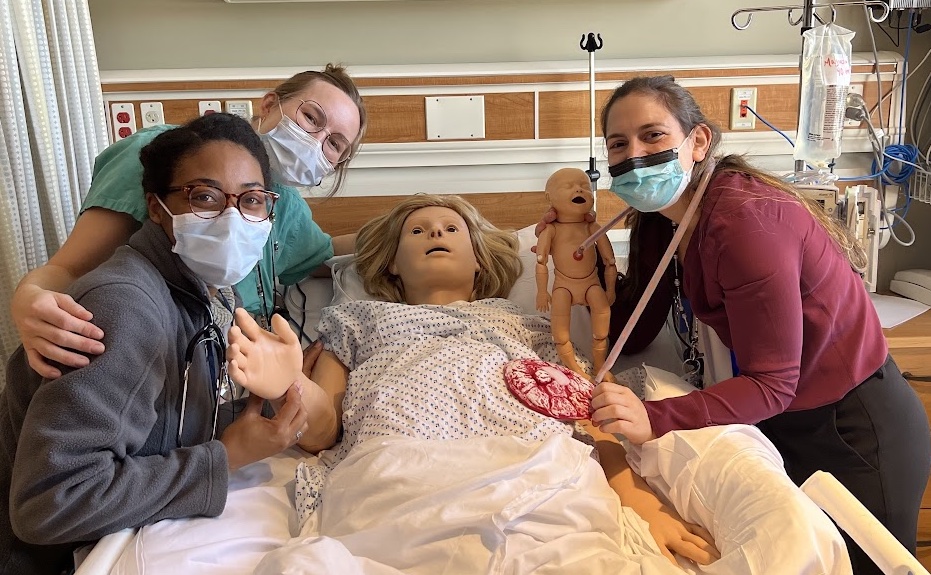

Intern Bootcamp: Two days of hands-on simulation training for incoming interns
Topics included in this curriculum are:
- Normal Labor
- Fetal Heart Rate Monitoring
- Introduction to the Operating Room
- Critical Anatomy for Gynecologic Surgeons
- Introduction to Surgical Instruments
- Vaginal Delivery Simulation
- Perineal Repair Simulation
- Cesarean Section Simulation
Obstetrics & Gynecology Core Simulation Curriculum
- Electrosurgery Bootcamp
- Obstetric and Gynecologic Ultrasound Simulation
- Family Planning Simulation
- LARC Insertion Certification
- MVA, D&C, D&E Simulation
- Laparoscopic Surgery Simulations
- Adnexal Surgery
- Myomectomy
- Sacrocolpopexy
- Pelvic Anatomy Simulation
- Hysteroscopy & Cystoscopy Simulation
- Hysterectomy Training
- Abdominal
- Laparoscopic
- Vaginal
- FLS & EMIGS Training
- DaVinci Robotic Simulation Training
- Colposcopy, LEEP, and CKC Simulation
- Pelvic Organ Prolapse Simulation
- Obstetric Hemorrhage
- Obstetric Hypertension Simulation
- Operative Vaginal Delivery Simulation
- Shoulder Dystocia Simulation
- 3rd and 4th Degree Laceration Simulation
Resident Wellness
The provision of competent, complex care in the high-stakes environment of Obstetrics & Gynecology and its subspecialties requires physician resiliency and attention to life inside and outside of medicine. Emotional and physical exhaustion must never displace the joy in medicine and managing the common stressors encountered during one’s professional career and personal life. Our residency program prioritizes initiatives that assess, promote, and maintain wellness amongst our residents and faculty. The Obstetrics and Gynecology Residency at Westchester Medical Center and Metropolitan Hospital provides patient centered care in a clinical learning environment founded in constructive behaviors of the physician workforce. The residency provides a platform on which residents develop the skills and attitudes needed to advance meaning in their career. This is accomplished through the teaching of skills to promote resiliency, enhance physician well-being, and combat burnout during residency and beyond. In collaboration with Westchester Medical Center as the Sponsoring Institution, the Obstetrics and Gynecology Residency Program has systems in place to monitor resident well-being, by balancing time with patients and personal time, mitigating non-physician obligations, optimizing clinical and administrative support, and the provision of resources for the support of clinician well-being.

Wellness Curriculum
- Readiness for Residency Curriculum
- Clinical Leadership Curriculum
- Community Service & Wellness Curriculum
- ACOG Residency Wellness Week
- Regular Wellness Activities – Organized by our Wellness Residents (resident selected)







Mentorship and Advisory Program
Our Mentorship & Advisory program is designed to provide each resident with a compatible mentor to serve in an advisory capacity regarding self-assessment and goal development.
Goal: Assist residents in their professional development through the guidance and support of experienced Department of OB/GYN faculty members who serve as role models, advisors, and advocates.
Structure: Faculty meet with their assigned mentee twice annually. This session includes review of their rotation evaluations, updates on their research, exam preparation, and fellowship and/or career planning.
Buddy System: All of the residents are paired with another resident from a different year to function as a mentorship buddy. Maintaining friendships and relationships within the residency program helps our residents work together through challenges and celebrate successes.

2024-2025 Obstetrics and Gynecology Residency at Westchester Medical Center
Quick Links:
Current Residents
PGY 4

Autumn Brewer, MD
Hometown: Sulphur Springs, TX
Undergraduate School: University of Mary Hardin-Baylor, Belton, TX
Medical School: Texas A&M College of Medicine, Temple, TX
Areas of Interest (OBGYN): Maternal Fetal Medicine, bridging healthcare disparities & increasing access to women’s healthcare, medical education
Hobbies: Taking Stella (my mini Aussie) on walks around Central Park, baking scones from scratch, traveling around the world, reading the newest novel/memoir, propagating house plants, sending snail mail, finding the best local happy hour specials, exploring all of NYC by foot & Citi Bike
Why NYMC: Early on in the residency search, I made a list of what I was looking for: a small-knit community of residents who feel like family, incredibly high acuity and patient pathology to prepare me for an MFM fellowship, diversity in patient populations and diversity in faculty/peers, strong focus on building bridges across healthcare disparities in the community, and a new city with opportunities to grow & explore with my pup. NYMC checked all of these boxes AND I get to live in NYC – truly a dream come true.

Cindy Coots, MD
Hometown: Autstin, TX
Undergraduate School: University of Texas, Austin, TX
Medical School: University of Texas, Houston, TX
Areas of Interest (OBGYN): Still very undecided because I just love it all. Possibly MIGS, MFM, Gyn Onc, or becoming an Academic Generalist!
Hobbies: Pretty much anything you can do outside! Hiking and rock climbing, long-distance running. I also knit and sew, and I love languages and literature!
Why NYMC: So many reasons!! Lots of subspecialty exposure, diverse and underserved patient population, high acuity cases, and seriously wonderful co-residents and faculty mentors.

Mariya Ledoux, MD
Hometown: Brooklyn, NY / Abakan, Russia
Undergraduate School: Boston University in Boston, MA
Medical School: Frank H. Netter MD School of Medicine at Quinnipiac in North Haven, CT
Areas of Interest (OBGYN): FPMRS, female sexual dysfunction, medical education, primary care, physician wellness
Hobbies: Distance running, destination cycling, skiing, live music, road trips, outdoors in every shape and form, spending time with my growing family, and throwing dinner parties
Why NYMC: I chose NYMC because I felt unparalleled welcome and warmth on my interview day. I was excited to meet and work with many of the mentors and faculty and to work with a diverse patient population in two different hospitals in NY. I'm also excited to work alongside such an amazing cohort of co-residents.

Rachel Zeuner, MD
Hometown: NYC
Undergraduate School: Washington University, St. Louis, MO
Medical School: Albert Einstein College of Medicine, Bronx, NY
Areas of interest: Gyn onc, gyn surgery, medical education, policy/advocacy, health equity
Hobbies: Gluten free baking, crafting, running, hosting friends for elaborate dinners, and traveling
Why NYMC: I’m excited to learn from patients in two different practice setting and to work with a great group of co-residents and a supportive faculty! And of course, I can’t wait to become an OBGYN in my favorite city!
PGY3

Alexa Leib, MD
Hometown: New York, NY
Undergraduate School: Davidson College, Davidson, NC
Medical School: Lewis Katz School of Medicine at Temple University Philadelphia, PA
Areas of interest: Addiction medicine, family planning, maternal fetal medicine, medical education and resident wellness
Hobbies: Trying new restaurants, visiting museums, traveling the world (collecting snow globes along the way), spending time with family and friends and dancing around my apartment.
Why NYMC: I loved the program because I get to work at two hospitals and learn to serve a patient populations! The people!! The fervor, passion, camaraderie and support within the department is unparalleled! Lastly I love NYC and Westchester - I am thrilled to become an OBGYN in the places I love.
Emily Passarelli, MD
Hometown: Rockville Centre, NY
Undergraduate School: Brown University, Providence, RI
Medical School: Warren Alpert Medical School of Brown University, Providence, RI
Areas of interest: FPMRS, trauma-informed care, medical education
Hobbies: loving my long-haired mini-dachshund, caring for my family of houseplants (and giving friends unsolicited advice on how much they should water their own plants), hiking new national parks, crocheting/embroidering/cross-stitching, begging my fiancé to come on long runs with me.
Why NYMC: The opportunity to train at a program where you can both directly serve the underserved and feel the benefit of a large academic center for research and to see higher-acuity, complex cases is amazing. Also, everyone was also so welcoming on interview day - choose your program based on where you think you have found your people.

Shirley Qian, MD
Hometown: Queens, NY
Undergraduate School: Macaulay Honors College - CUNY Hunter College, New York, NY
Medical School: SUNY Downstate College of Medicine, Brooklyn, NY
Areas of interest: Urogyn, gyn surgery, patient education & advocacy, health equity - I am really excited to explore all the subspecialties and keeping my mind open to the possibilities!
Hobbies: Baking, cooking, hiking, travel, spending quality time with friends & family
Why NYMC: I fell in love with the program on my interview day. It has everything I’m looking for in a residency program - commitment to patient advocacy and serving underserved communities, diversity in pathology, acuity, and patient population, and supportive faculty and residents.

Olivia Recabo, MD
Hometown: Yorktown, NY
Undergraduate School: Brown University, Providence, RI
Medical School: Warren Alpert Medical School of Brown University, Providence, RI
Areas of interest: Still undecided! Possibly Gyn Onc, MFM, or becoming an Academic Generalist.
Hobbies: Weightlifting, anything and everything outdoors, feeding people my over-the-top baking creations, acrylic painting, traveling.
Why NYMC: I felt so welcomed by every single person I met on interview day that I knew I would be able to find close friends and mentors during my four years here. I was really excited about the ability to care for diverse patient populations at two different hospitals, and even more thrilled that one of them is in NYC while the other is so close to home. I knew that NYMC would be a fantastic place to explore my passions within Ob/Gyn and that I would leave residency well-prepared for any career I choose.
PGY2

Brenda Lubochiner, MD
Hometown: Buenos Aires, Argentina
Undergraduate School: University of Buenos Aires, Argentina
Medical School: University of Buenos Aires, Argentina
Hometown: Buenos Aires, Argentina
Undergraduate School: University of Buenos Aires, Argentina
Medical School: University of Buenos Aires, Argentina
Areas of interest: Family Planning, MIGS
Hobbies: Walking my dog Floyd, watching The Office, reading a book, cleaning & organizing, cooking.
Why WMC: People who you can tell are awesome to work with (number 1 reason!) + diversity of patient population + women's rights are respected.

Benjamin Rabinowitz, MD
Hometown: Merrick, NY
Undergraduate School: Vanderbilt University, Nashville, TN
Medical School: New York Medical College, Valhalla, NY
Areas of interest: REI, Urogyn, MIGS, LGBTQ+ health, reproductive justice, patient advocacy, resident wellness
Hobbies: I love playing soccer, pickleball, runs on the West Side Highway & Central Park, traveling, trying new restaurants in NYC, live music & dancing, and seeing Broadway shows and movies.
Why WMC: I chose NYMC because it has so much to offer. Providing comprehensive care to a diverse patient population at both an academic center and community hospital in NYC. The wonderful faculty and residents that have made me feel at home and part of a family when I was a medical student. The opportunity to explore all the different subspecialties in OB/GYN and leave residency ready to take on any path I choose.

Ashley Silver, MD
Hometown: Cortlandt Manor, NY
Undergraduate School: Cornell University, Ithaca, NY
Medical School: University of Virginia, Charlottesville, VA
Hometown: Cortlandt Manor, NY
Undergraduate School: Cornell University, Ithaca, NY
Medical School: University of Virginia, Charlottesville, VA
Areas of interest: General OB-GYN, reproductive health education and advocacy, family planning
Hobbies: Yoga, cooking, exploring new countries, trying new restaurants, spending time with friends and family
Fun Fact: I had a very close encounter with a bear and her cubs while hiking...maybe that's why hiking isn't listed under my hobbies
Why WMC: I wanted the opportunity to train at two very different hospitals so I could be prepared to care for any and all patients, including underserved, culturally diverse, and high-acuity patients. I also felt incredible support and excitement from faculty on my interview day, and knew this was an environment that would foster my learning and growth.
Melissa Yuce, MD
Hometown: Greensboro, NC
Undergraduate School: Wake Forest University, Winston-Salem, NC
Medical School: Wake Forest University School of Medicine, Winston-Salem, NC
Hometown: Greensboro, NC
Undergraduate School: Wake Forest University, Winston-Salem, NC
Medical School: Wake Forest School of Medicine, Winston-Salem, NC
Areas of interest: Health equity, family planning, global and rural health
Hobbies: I like playing volleyball (grass, beach, or indoor), hiking, doing puzzles while drinking coffee and watching my current TV show (my largest puzzle was 3,000 pieces!), listening to podcasts, spending time with family and hanging out with my husband and our dog.
Why WMC: I really value an environment where everyone supports each other in their personal and professional goals, and NYMC reflected that value for me. I also love the diverse populations that this program serves as someone who hopes to provide bilingual services to my patients.
PGY1

Eva Chorna Sherman, MD
Hometown: Buenos Aires, Argentina
Undergraduate School: University of Buenos Aires, Argentina
Medical School: University of Buenos Aires, Argentina
Hometown: Paris, France
Undergraduate School: McGill University Montreal, Canada
Medical School: New York Medical College
Areas of interest: All of ObGyn, access to healthcare and health equity
Hobbies: Travelling to different countries, skiing, swimming, reading, and spending time with my family
Why WMC: I love this program because there is a great breadth of exposure to unique pathology and cases in all areas of ObGyn, there is a diverse patient population, and above all an incredible group of co-residents and attendings to train alongside in an environment of constant learning and growth.

Tiffany Fanning, MD
Hometown: Buenos Aires, Argentina
Undergraduate School: University of Buenos Aires, Argentina
Medical School: University of Buenos Aires, Argentina
Hometown: Buchanan, NY
Undergraduate School: Columbia University - New York, NY
Graduate School: Columbia University - Mailman School of Public Health New York, NY
Medical School: Zucker School of Medicine Hofstra/Northwell
Areas of interest: General obgyn, reproductive justice, family planning, health equity
Hobbies: Walking my dog, skiing, spending time with family, watching re-runs on TV
Why WMC: Having lived in Westchester for the majority of my life, I wanted to give back to a community I have loved being part of. I wanted to work with a diverse population, with faculty who cared about my growth and development as a physician and an individual, and with co residents who would support me on my own residency journey.

Colleen Livingston, MD
Hometown: Buenos Aires, Argentina
Undergraduate School: University of Buenos Aires, Argentina
Medical School: University of Buenos Aires, Argentina
Hometown: Dallas, TX
Undergraduate School: Texas A&M University College Station
Medical School: McGovern Medical School at UT Houston
Areas of interest: Gyn oncology, reproductive justice & patient advocacy, contraceptive counseling and education, family planning, LGBTQ+ health
Hobbies: Matcha (I make the best matcha latte to ruin all coffee shop matcha lattes), sand volleyball, boxing/shadow boxing, watching reality TV (all things Bravo and Love Island are my current favs)
Why WMC: I wanted to train in an environment that prioritizes and values the growth and education of its residents from the top-down. Even from my first interactions, I felt supported and respected by the NYMC faculty and other residents. I could tell that everyone genuinely loved being part of this program and providing care for the patients of Westchester and East Harlem. Bonus points because clinical experiences at Westchester are truly unmatched! You've heard the saying "when you hear hoofbeats, think horses not zebras" but at Westchester, be prepared for the zebras!
Dena Phillips, MD
Hometown: Buenos Aires, Argentina
Undergraduate School: University of Buenos Aires, Argentina
Medical School: University of Buenos Aires, Argentina
Hometown: Seattle, WA
Undergraduate School: Yeshiva University New York, NY
Medical School: New York Medical College
Areas of interest: Generalist
Hobbies: Reading, exercise, yoga, TV, spending time with friends!
Why WMC: The community at WMC is unmatched, the residents all really love each other and that kind of support is exactly what I was looking for in a residency! The opportunities and growth at this program also really impressed me, and I know I will be able to explore my potential here.

Alyssa Sheedy, MD
Hometown: Buenos Aires, Argentina
Undergraduate School: University of Buenos Aires, Argentina
Medical School: University of Buenos Aires, Argentina
Hometown: Buffalo, New York
Undergraduate School: Cornell University Ithaca, New York
Medical School: Jacobs School of Medicine at University of Buffalo
Areas of interest: Urogynecology, MIGS, medical education, health equity
Hobbies: Yoga, indoor cycling, skiing, traveling, watching reality TV, cheering for the Buffalo Bills, spending time with my family and friends!
Why WMC: I fell in love with the program on my interview day! Working amongst supportive, passionate, and hard-working faculty and residents who champion one another to foster camaraderie and mentorship is something I really value. Also, having the opportunity to train at two very different hospitals with diverse patient populations, high-acuity care and cases that span all the fields within OBGYN is truly incredible
Our Faculty at Westchester Medical Center
Julia Keltz, MD
Residency Program Director,
Clinical Assistant Professor,
Attending Physician
- Obstetrics & Gynecology
- Obstetrics & Gynecology, Minimally Invasive and Gynecological Surgery
Sean Tedjarati, MD
Chair & Clinical Professor/Director,
Department of Obstetrics and Gynecology
- Obstetrics & Gynecology, Gynecologic Oncology
- Obstetrics & Gynecology, Gynecologic Oncology
- Urology, Neuro Urology & Voiding Dysfunction
- Urology, Female Pelvic Medicine and Reconstructive Surgery
- Obstetrics & Gynecology
- Obstetrics & Gynecology, Gynecology
- Obstetrics & Gynecology, Minimally Invasive and Gynecological Surgery
- Obstetrics & Gynecology, Obstetrics
- Obstetrics & Gynecology, Maternal & Fetal Medicine
- Obstetrics & Gynecology
- Obstetrics & Gynecology, Female Pelvic Medicine and Reconstructive Surgery
Martin Keltz, MD
Attending Physician, Director of Reproductive Endocrinology and Infertility, WestMed
- Obstetrics & Gynecology, Reproductive Endocrinology
- Obstetrics & Gynecology
- Obstetrics & Gynecology, Gynecology
- Obstetrics & Gynecology, Female Pelvic Medicine and Reconstructive Surgery
- Obstetrics & Gynecology
- Obstetrics & Gynecology, Maternal & Fetal Medicine
Akiva Novetsky, MD
Attending Physician
Medical Director of Quality and Safety for the Department of Obstetrics and Gynecology
- Obstetrics & Gynecology
- Obstetrics & Gynecology
- Obstetrics & Gynecology, Female Pelvic Medicine and Reconstructive Surgery
Tana Pradhan, DO
Chief, Division of Gynecologic Oncology and Robotic Gynecologic Surgery
- Obstetrics & Gynecology, Gynecologic Oncology
- Obstetrics & Gynecology, Maternal & Fetal Medicine
- Pediatrics, Pediatric Gynecology
- Obstetrics & Gynecology, Minimally Invasive and Gynecological Surgery
- Obstetrics & Gynecology
- Obstetrics & Gynecology
- Pediatrics, Pediatric & Adolescent Gynecology
Brittany Sanford, MD
Attending Physician, Assistant Director of Labor and Delivery; Assistant Professor, New York Medical College
- Obstetrics & Gynecology, Maternal & Fetal Medicine
- Obstetrics & Gynecology
Bianca Stifani, MD
Associate Medical Director, Complex Family Planning Attending Physician
- Obstetrics & Gynecology
- Obstetrics & Gynecology, Minimally Invasive and Gynecological Surgery
Ming Tsai, MD
Clinical Professor, Associate Director, Department of Obstetrics and Gynecology, Westchester Medical Center, New York Medical College
Director of Quality and Safety, WMCHealth Physicians, Advanced Physician Services
- Obstetrics & Gynecology
- Obstetrics & Gynecology, Maternal & Fetal Medicine
Our Faculty at Kingston
Our Faculty at NYC Health + Hospitals/Metropolitan
Advanced Urogynecology

Vani Dandolu, MBBS
Chairperson
Department of Obstetrics and Gynecology
Maternal Fetal Medicine Division

Jonathan K. Mays, MD, MPH, MBA, FACOG
Deputy Director of Obstetrics and Gynecology
Attending Physician
MIGS Division

Pavan K. Ananth, MD
Attending Physician
Generalist Division

Elmer C. Agustin, MD, MPH, FACOG
Director, Colposcopy & Dysplasia
Attending Physician
|

Cornea N. Khan, MD
Attending Physician
|
Gladys M. Lee-Hwang, MD, FACOG
Director of Labor and Delivery
Attending Physician
|

Michele M. Paolucci, MD, FACOG
Attending Physician
|

Joseph D. Santoro, MD, FACOG
Director of Gynecology
Attending Physician
|

Setareh Shams, MD, FACOG
Attending Physician
|

Alexander Shilkrut, DO, FACOG
Attending Physician
|
Angelica Sze, MD, FACOG
Associate Program Director
Attending Physician
|

Sorana Vrabie-Wolf, MD, FACOG
Attending Physician
|
|
|
|
Physician Assistants and Staff
Division of Gynecologic Oncology and Robotic Gynecologic Surgery
Division of General Obstetrics and Gynecology
Maternal-Fetal Medicine Division
Minimally Invasive Gynecologic Surgery, Complex Family Planning, and Urogynecology Division
Our Staff at Kingston

Megan Corjulo, CNM
Nurse Midwife
|

Bethany Grimes, CNM
Nurse Midwife
|

Elissa Marsh, CNM
Nurse Midwife
|
Department Administration
Westchester Medical Center
|

Coral Matar, MPA
Administrative Director
|

Melisa Cerpa
Program Manager
|

Blanca Rodriguez, MA
Quality Manager
|

Jessica Berrios-Elliott, MIS, C-TAGME
Residency Manager
|
 |
|
|
|
Lisette Alvarez, LMSW
Network Senior Social Worker |
|
|
|
New York Medical College
|

Bruno S. Villazhiñay Matute, MPH., Dr.P.H.(c)
Senior Administrator
|
NYC Health + Hospitals/Metropolitan
|

Beverly Fishburne
Residency Coordinator
|
Program Alumni
2024
Maria Morgan, MD: Pediatric and Adolescent Gynecology Fellowship at The Hospital for Sick Children/University of Toronto
Amythis Soltani, MD: Complex Family Planning Fellowship at Stanford University Health Care
Katya Wentzel, MD: Minimally Invasive Gynecologic Surgery Fellowship at Yale New Haven Health
Helen Zhang, MD: Female Pelvic Medicine and Reconstructive Surgery Fellowship at Medstar Health
2023
Alborz Borjian, DO: Attending, Facey Medical Group - Providence, California
Sapphire Holness, MD: Attending, Phelps Hospital Sleepy Hollow, NY
Bernice Li, MD: Attending, Maimonides Medical Center, Brooklyn, NY
Julia Youssef, MD: Attending, Inspira Medical Center, Mullica Hill, NJ
2022
Sarah Kwarteng Peprah, MD: Attending, Columbia Doctors NYP – Lawrence Hospital, Bronxville, NY
Melanie Peters, MD: Attending, Downstate University Hospital, Brooklyn, NY
Miriam Toaff, MD: Attending, Premium Health, Brooklyn, NY
Sarah Weingarten, MD: Maternal Fetal Medicine Fellowship, Weill Cornell, New York, NY
2021
Itamar Futterman, MD: Maternal Fetal Medicine Fellowship, Maimonides Medical Center, Brooklyn, NY
Emily Rosenfeld, DO: Maternal Fetal Medicine Fellowship, Robert Wood Johnson/Rutgers, New Brunswick, NJ
Nidhi Shah, MD: Attending, Jamaica Hospital Center, Queens, NY
Rayna Trietsch, MD: Attending, Women's Health Care Associates, Littleton, CO

WMC has officially launched Graduway, an Alumni Platform. Visit WMC Alumni online.
The Alumni Connection provides a professional social network for graduates of our Residency and Fellowship Programs to reconnect with former colleagues and mentors as well as be informed about professional opportunities at the WMC Health Network.