Welcome From the Program Director
Welcome and thank you for your interest in Westchester Medical Center Health Network's newly established ACGME-accredited categorical four-year residency training program in Physical Medicine and Rehabilitation. We are committed to providing a diverse, inclusive, and supportive learning environment in which our trainees not only succeed but can excel. WMC PM&R's goal is to provide residents with comprehensive training and education in all aspects of the practice of PM&R. We have recruited outstanding faculty mentors, designed our clinical rotations to provide a strong foundation in clinical skills, and developed an extensive educational curriculum that includes weekly lectures and seminars, journal clubs, case conferences, written board reviews, and a regular MSK and neuroradiology series. We also offer an excellent resident wellness program and individualized mentoring program.
WMC is a tertiary/quaternary care hospital, level one trauma center, primary stroke center, burn center, and houses the Brain and Spine Institute. WMC sponsors 17 ACGME-accredited residencies and 24 advanced fellowships. A major teaching affiliate of New York Medical College (NYMC) and co-located on the Valhalla academic campus, WMC PM&R residents assist in the teaching of students completing their required third year clerkship in PM&R as well as students enrolled in our fourth-year student electives. The academic campus affords residents the opportunity to collaborate with a host of other academic programs. The NYMC School of Health Sciences and Practice offers degree programs in Physical Therapy and Speech Language Pathology and also houses the Centers on Disability and Health, Medical Outcomes Research, and Long-Term Care. Other outstanding resources on the NYMC campus include a clinical skills and simulation center, the anatomy dissection lab, and the Westchester Institute for Human Development (WIHD). WIHD provides primary care and rehab services to over 5,000 persons with disabilities.
Our graduates obtain the strong educational foundation necessary to enter the next step of their careers, whether it be subspecialty fellowship training, private practice, or academic medicine. Our diverse and highly trained faculty provide mentorship and guidance in a positive and supportive environment that allows our residents to grow as caring and compassionate physicians. We are committed to the success of our graduates and proud of the incredible training opportunity our program offers.
Paul T. Diamond, MD
Director and Chief of Service
Residency Program Director
Professor
Medical School: University of Virginia
Residency (IM): Johns Hopkins Medical Institutions
Residency (PM&R): Sinai Rehabilitation Center / Johns Hopkins
WMC Residency Training Program at a Glance
- A four-year ACGME-accredited categorical residency in PM&R
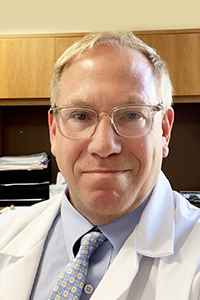
- The PGY-1 year or intern year includes 35 weeks of internal medicine, five weeks of neurology, two weeks of pain management, two weeks of orthopedic/MSK radiology and four weeks of PM&R.
- The total number of resident positions is 16 with four residents per training year
- The primary training site and sponsor of the program is Westchester Medical Center Health Network, a major teaching affiliate of New York Medical College.
- Affiliated training sites include MidHudson Regional Hospital,James J. Peters VA Medical Center, and Blythedale Children's Hospital.
- For the 2025 NRMP, WMC PM&R will be offering four PGY1 positions for enrollment in July 2025.
- After the internship year, residents provide on call coverage from home.
Mission
The mission of the Westchester Medical Center Health Network Physical Medicine & Rehabilitation Residency Program is to provide our residents with the knowledge and skills necessary to be highly competent and compassionate physiatrists, prepare them for careers of lifelong learning, and demonstrate, through example, the importance of character and professionalism in the delivery of healthcare. We teach our residents to advocate for their patients, especially the most vulnerable with limited resources, in a variety of clinical settings and communities so that every patient can receive the healthcare and support they need to recover to the fullest extent possible.
Program Aims
Residents gain experience in a broad range of clinical settings and subspecialty areas to fully prepare them for independent clinical practice. Although the primary training site is an academic tertiary care level one trauma center, residents also rotate through a community hospital-based general rehabilitation unit and outpatient practice, a VA-based SCI specialty service, a secure brain injury unit in a free-standing rehabilitation hospital, a pediatric specialty care hospital, and a community-based subacute rehabilitation unit. Residents also train in a variety of outpatient clinical settings including the WMC-based interventional spine / musculoskeletal medicine clinics, the sports medicine clinic, prosthetics and orthotics clinic, electrodiagnosis clinic, cancer survivorship and general rehabilitation clinics and spasticity clinic, Blythedale Children’s Hospital’s pediatric day treatment clinic and adaptive/assistive/WC seating clinic, and the VAMC’s SCI, MS, and ALS clinics. Each of these experiences exposes residents to unique patient populations with varying needs and resources, so critical to their training. Our faculty serve as role models for professionalism, clinical acumen, and patient advocacy as they mentor our residents throughout their four years of PM&R training. The goal of our program is to prepare our graduates to be highly informed and compassionate physicians providing the highest level of physiatric care to their patients.
Clinical Rotations
PGY-1 Rotations
This year is designed to provide a strong foundation in medical management while also introducing residents to some of the disciplines they will be closely collaborating with throughout their residency and as practicing physiatrists. The PGY-1 year is an integral part of the four-year categorical residency program. PGY-1 residents are assigned a PM&R faculty mentor and upper level resident advisor. PGY-1 residents participate in the monthly program directors’ meetings and are invited to attend all PM&R educational activities and events. The PM&R program director meets with each resident individually for their semiannual performance evaluations.
Internal Medicine – 35 weeks
- General Medicine Floors – 18 weeks
- Ambulatory Care – 2 weeks
- Electives (specialty consults) – 10 weeks
- Admitting Consult Team – 2 weeks
- Night Floats – 3 weeks
Neurology Stroke and Hospital Service – 3 weeks
Neurology Outpatient Clinics – 1 week
Neurological ICU – 1 week
Pain Management (interventional / OP / consults) – 2 weeks
Orthopaedics Clinics / MSK Radiology – 2 weeks
PM&R Inpatient – 2 weeks
PM&R Outpatient – 2 weeks
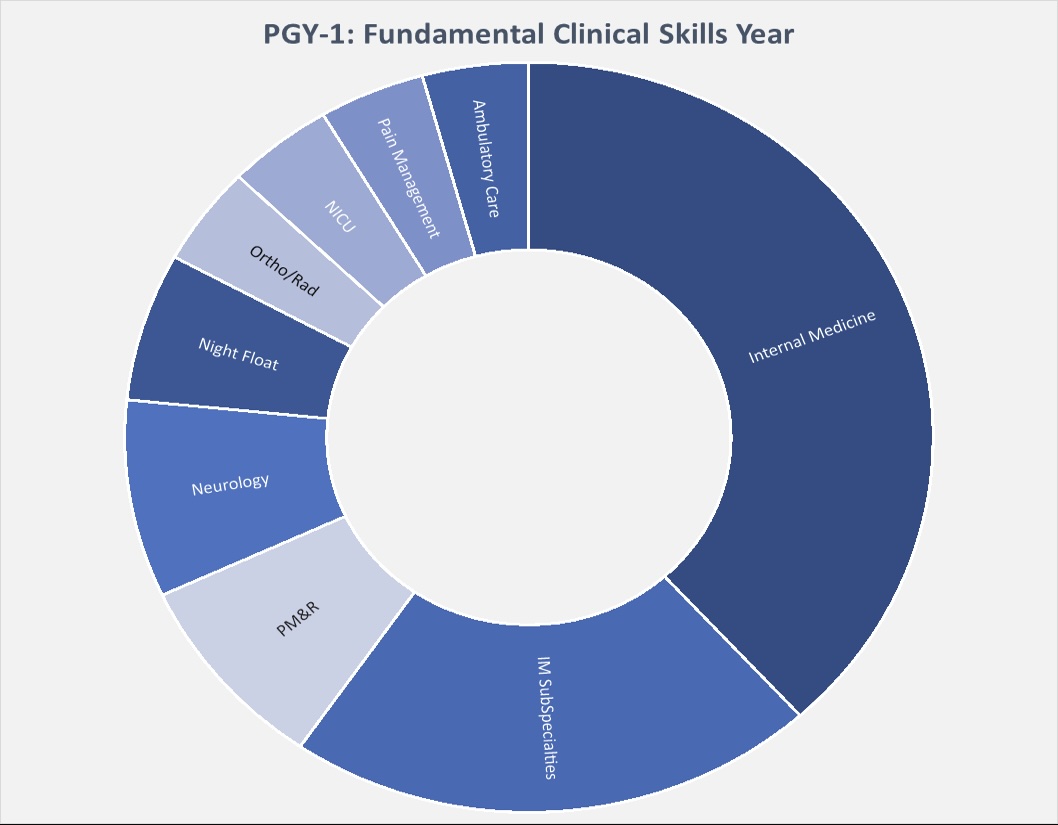
PGY-2 Rotations
This year is designed to provide residents with the competencies required to manage patients both medically and from a rehabilitation perspective during inpatient rehabilitation care. A one-month elective is also offered to allow residents to begin to explore areas of particular interest early on in their training. Rotations sites include the general inpatient rehabilitation service at Westchester Medical Center (WMC), the acquired brain injury (ABI) service at Burke Rehabilitation Hospital, and the SCI rehabilitation service at the James J. Peters VAMC.
- General Inpatient Rehabilitation at WMC – 9 months
- Acquired Brain Injury at Burke – 1 month
- SCI Rehabilitation at VAMC – 1 month
- Elective – 1 month
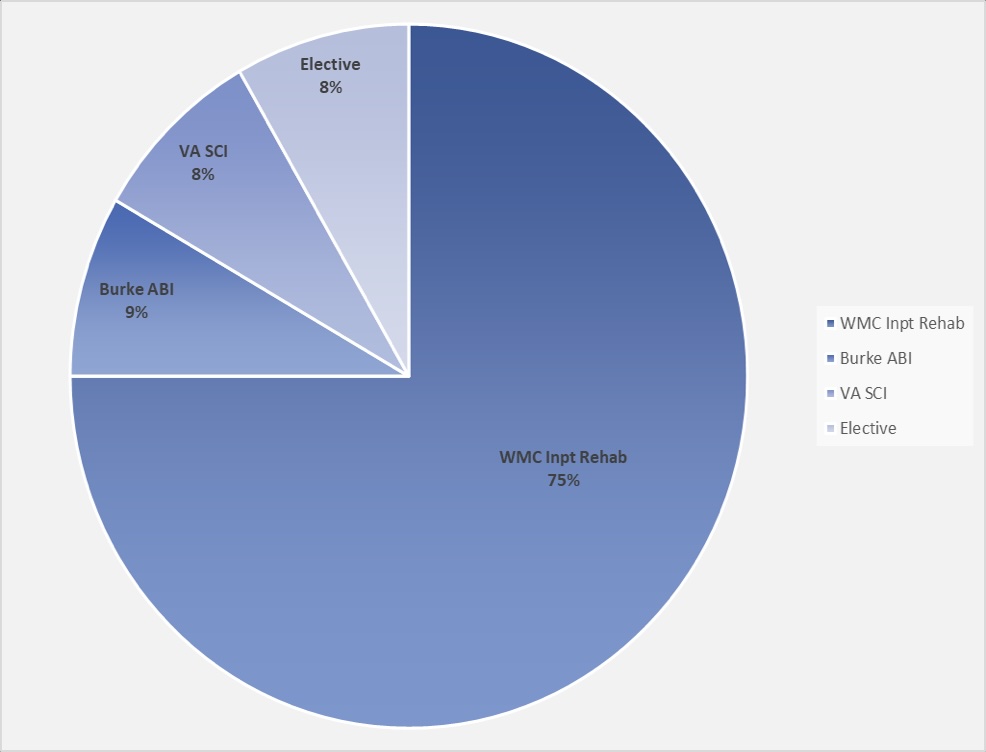
PGY-3 Rotations
This year is designed to provide residents with exposure and training in a variety of clinical outpatient settings. Residents rotate through the PM&R specialty practices, including the spine and sports medicine clinics, spasticity clinic, and neuro/general rehab clinic. Residents complete their two preliminary training months in electrodiagnosis. They rotate through the cardiopulmonary and prosthetics / orthotics services and complete their rotation in subacute geriatric rehabilitation at The Grove Rehabilitation and Nursing Center. Residents spend one month at Mid-Hudson Regional Hospital working with physiatrists on both the inpatient and outpatient services. While at the Blythedale Children's Hospital, residents rotate through the pediatric orthotics clinic, assistive and adaptive equipment clinic, and wheelchair seating clinic as well as the outpatient day treatment program. At the Maria Fareri Children’s Hospital residents see outpatients and consults with the pediatric physiatry team. In addition, residents have a one-month clinical elective during the PGY-3 year.
- PM&R Outpatient Clinics – 4.5 months
- Electrodiagnosis Lab – 2 months
- Cardiac Rehab / Subacute Rehab – 2 weeks
- Mid-Hudson Regional Hospital – 1 month
- Maria Fareri Children's Hospital – 2 months
- Blythedale Children's Hospital – 1 month
- Clinical Elective – 1 month
PGY-4 Rotations
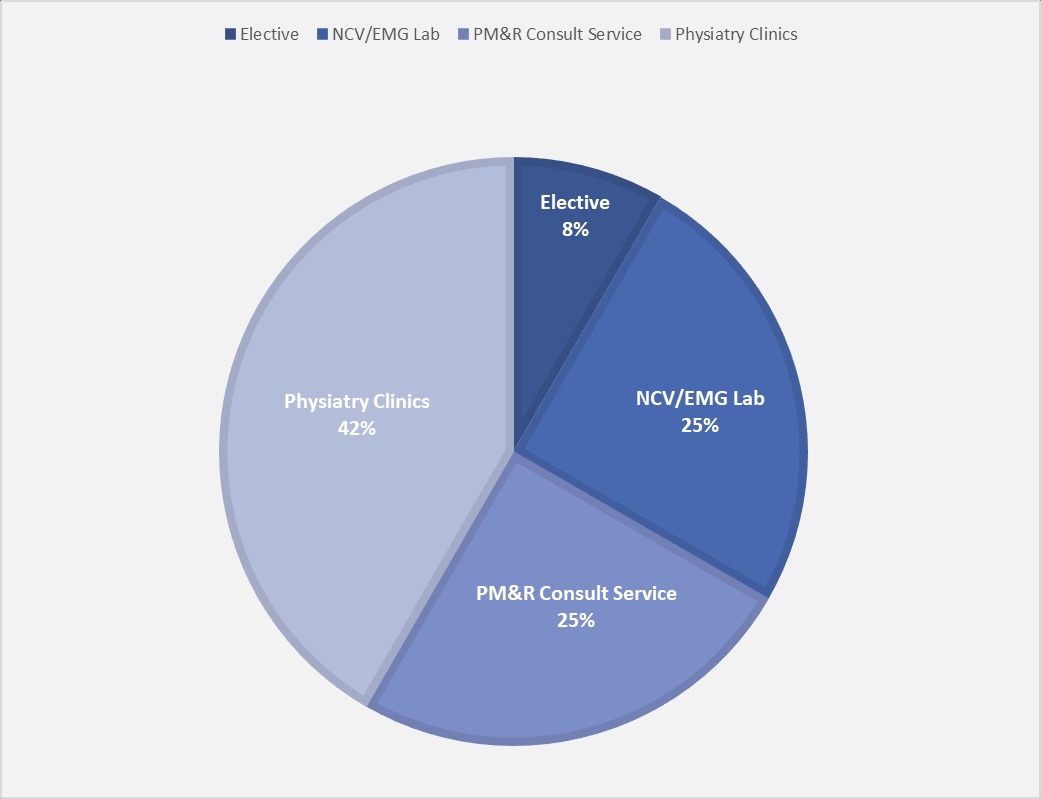
The senior year of residency is the final stage in providing graduates of our program with the knowledge, skills and professionalism necessary for autonomous practice. Senior residents serve in supervisory roles over more junior residents in the outpatient clinics and electrodiagnosis lab, complete their log of procedures required to qualify for board certification in PM&R, and provide consultative services throughout the hospital under the supervision and guidance of the consult attending.
- PM&R Outpatient Clinics – 5 months
- Electrodiagnosis Lab – 3 months
- PM&R Consult Service – 3 months
- Elective – 1 month
Educational Curriculum
A comprehensive educational curriculum has been established to complement the clinical rotation curriculum. The curriculum has multiple facets and includes a core lecture series held weekly and organized topically. Core teaching faculty and guest faculty are assigned selected topics within each month's designated focus area. Residents are excused from clinical assignments to attend. To ensure attendance and protected educational time, attendings are assigned to cover all clinical services.
Core lectures: Grouped topically over a 12-month cycle as follows:
- Rehabilitation Principles – 4 weeks
- Professionalism, Systems of Care, Public Health and Clinical Research – 4 weeks
- Neurorehabilitation and SCI – 8 weeks
- Amputations, Prosthetics / Orthotics – four weeks
- Disease-Specific Rehabilitation: Cancer; Burn; Cardiopulm; Geriatric; Rheum – 4 weeks
- Pain Principles and Management – 4 weeks
- Musculoskeletal / Spine and Sports – 8 weeks
- Principles of Electrodiagnosis and Neuromuscular Syndromes – 8 weeks
- Pediatric Rehabilitation – 4 weeks
Grand Rounds: Held monthly, nationally and internationally recognized speakers present on a variety of rehabilitation-related topics of broad interest. Grand rounds are multidisciplinary and can be viewed remotely or in-person.
Journal Club: Journal club is held twice each month. The chief resident assigns residents in advance who select a peer-reviewed journal article for critical review. The attending assigned as the journal club preceptor approves the article and/or makes recommendations for articles for presentation.
Radiology Rounds: At radiology rounds, residents learn to read a variety of radiographic films under the supervision of PM&R attendings and radiologists. Sessions alternate between musculoskeletal radiology and neuroradiology. Several MSK ultrasound sessions are included in this educational series.
Challenging Cases: Case conference is held monthly and coordinated by the program director. Residents are invited to present a particularly challenging case for discussion and assigned a faculty member to assist them with preparing their presentation. All faculty and residents are encouraged to attend.
Anatomy Lab: Six anatomy lab sessions are held annually in the Cadaver lab on the Valhalla campus of Westchester Medical Center and New York Medical College (NYMC). Anatomy instruction is provided by the NYMC Department of Anatomy Faculty and specifically focuses on clinically relevant musculoskeletal and peripheral nerve anatomy. These sessions are supplemented by lectures given by the clinical faculty to highlight the application of the basic anatomy to the clinical practice of PM&R.
Research Day: Residents are encouraged to participate in research and prepare abstracts for presentation at the AAP and AAPM&R meetings. Research day is held annually and is an opportunity for residents and faculty to showcase their research to the entire department and prepare their posters for formal presentation.
AMA GME Competency Education Program (GCEP): Residents complete the following online courses for professional development: Residents as teachers; Managing Unconscious Bias; Creating an Effective and Respectful Learning Environment; Patient Safety; Cultural Competency; Thriving Through Residency; Resident Intimidation; Sleep Deprivation; Patient Handoffs; Building the Patient-Physician Relationship; Using Tools to Form an Action Plan for Wellness; Health Care Quality: Measuring Physician Performance; Physician Health: Physicians Caring for Ourselves; Coding and Documentation; Safer Prescribing and Managing of Opioids.
Faculty Mentors: All residents are assigned or may select a faculty member to serve as their mentor. Residents meet with their faculty mentors regularly and work together to prepare their annual individualized learning plan (ILP): The ILP is used to help tailor each resident's experience to their own learning and career goals.
Program Evaluation Committee (PEC): The PEC consists of the program director, teaching faculty, and a resident representative from each training year. The committee meets monthly and serves as a residency advisory board for the department. The purpose of the committee is to maintain the highest quality of resident education and training.
Resident Retreats: Generally held quarterly, these group activities are part of a comprehensive resident wellness program. The Subcommittee on Resident Wellness meets monthly and is designed to discuss best practices for trainee wellness.
Preparation for the AAPM&R Boards: Preparation for written boards is facilitated through regularly scheduled board review sessions. Residents also take the AAPM&R sponsored Self-Assessment Exam (SAE) annually. Mock orals are held annually for the PGY3 and PGY4 residents by the program director and teaching faculty.
Memberships / Attendance at National Meetings
Resident receive annual memberships in the American Academy of PM&R (AAPM&R), Association of Academic Physiatrists (AAP), and New York Society of PM&R (NYSPM&R). Residents are encouraged to present research abstracts at professional meetings. Funding is available for air travel, three nights lodging, meals, and meeting attendance with preapproval.
Clinical Training Sites

Westchester Medical Center (WMC) is a 652-bed tertiary and quaternary acute care hospital, level 1 trauma center, burn center, comprehensive stroke center, and major teaching affiliate of New York Medical College (NYMC). Serving as the primary training site, WMC provides PGY-1 training in the fundamental clinical skills including internal medicine, emergency medicine, neurology, radiology and orthopedics. PGY-2 through PGY-4 training includes broad educational experiences in acute inpatient rehabilitation (18-bed unit), outpatient PM&R, sports medicine, neurorehabilitation, spasticity clinic, electrodiagnosis, interventional spine / musculoskeletal / pain clinic, cardiopulmonary rehabilitation and prosthetics/orthotics. WMC is the site of the didactics program, journal club, CME grand rounds, musculoskeletal and neuroradiology rounds, complex cases series, and board review series. The core anatomy lectures and lab sessions also occur on the combined WMC / NYMC Valhalla campus. A broad array of clinical research and elective opportunities are offered at WMC and in collaboration with the NYMC School of Health Sciences and Practice, which offers degree programs in physical therapy and speech language pathology and houses the Centers on Disability and Health, Medical Outcomes Research, and Long-Term Care.

MidHudson Regional Hospital (MHRH), one of 11 hospitals within the WMCHealth network, is a 243-bed acute care hospital and level II trauma center located in Dutchess County, NY, a designated medically underserved non-rural area. This site houses an 18-bed acute inpatient rehabilitation unit, an outpatient physiatry clinic, and an outpatient therapy center. Residents rotate through both the inpatient unit and outpatient physiatry clinic where they gain early exposure to electrodiagnosis, Botox injections and other clinic-based procedures. All WMC-based didactics are presented on a hybrid platform (remotely and in person) and therefore available for participation from this site.

The James J. Peters Veterans Affairs Medical Center (VAMC) is a 311-bed facility with a 48-bed acute inpatient rehabilitation service, located in Bronx, NY. It is named after James J. Peters, a US army veteran, who established several organizations that provide support for persons with spinal cord injury (SCI). Residents rotate through the SCI rehabilitation program, including a dedicated SCI inpatient unit, and receive training in the medical and rehabilitative management of this patient population. This educational experience is supplemented by participation in several of the specialty clinics including wheelchair seating clinic, neuromuscular disorders clinic, and prosthetics/orthotics clinic. The VAMC also houses a center of excellence in SCI research. Resident didactics are offered onsite. All WMC-based didactics are presented on a hybrid platform (remotely and in person) and therefore available for participation from this site.

Blythedale Children's Hospital (BCH) is a 118-bed specialty care children's hospital treating children with complex medical and rehabilitative needs. Fifteen beds are dedicated to pediatric inpatient rehabilitation. At BCH, residents rotate through an array of specialized pediatric rehabilitation services. Experiences include the pediatric rehabilitation unit, pediatric physiatry consult service, the day treatment hospital, the orthotics clinic, and the adaptive/assistive equipment and wheelchair seating assessment clinics. Residents participate in the extensive on-site didactics curriculum. All WMC-based didactics are presented on a hybrid platform (remotely and in person) and therefore available for participation from this site.

The Grove at Valhalla Rehabilitation and Nursing Center is a 160-bed nursing facility located minutes from WMC and houses two subacute rehabilitation units and two long term care units. Our PM&R residents gain valuable experience in subacute rehabilitation and how it differs from acute inpatient rehabilitative care. Residents round with the facility's geriatric specialist and medical director, attend team conferences, and observe subacute geriatric rehabilitative treatment approaches in the facility's expansive rehabilitation gym. All WMC-based didactics are presented on a hybrid platform (remotely and in person) and therefore available for participation from this site.
The NYMC gross anatomy lab is also located on the Valhalla campus and provides the residents training and education in anatomy through active dissection of cadavers, detailed examination of prosected specimens, and an anatomy didactics program.
The NYMC School of Health Sciences and Practice (SHSP) is located on the combined campuses of Westchester Medical Center and New York Medical College. SHSP houses a Physical Therapy doctoral program and Speech Language Pathology Master's program, a Bioethics Program, the Center on Disability and Health, and the Center for Long-Term Care. The mission of the Center on Disability and Health is to promote health and access to care for people with disabilities, prevent secondary conditions and eliminate disparities between people with and without disabilities. The Center for Long-Term Care conducts research, education, and public policy development designed to improve the quality of long-term care and address healthcare disparities, healthcare needs and caregiving, and to promote strategies for fair and equitable financing of long-term care. This center plays an important role in providing education and training specific to disparities in healthcare and access to healthcare.
The Westchester Institute for Human Development (WIHD) is also located on the combined campuses. WIHD's mission is to help persons with disabilities live healthy and productive lies as full members of society. Services include audiology, assistive technology, adaptive and assistive equipment, physical and occupational therapy, speech language pathology, psychology, dental, and primary care for over 5000 persons with disabilities.

Burke Rehabilitation Hospital is a 150-bed acute rehabilitation hospital located in Westchester County. Residents will receive training and education in the medical and rehabilitative care and management of patients with traumatic brain injury on the secure 30-bed TBI unit. Clinical and teaching rounds will focus on assessment tools, neurobehavioral management, complications of TBI such as spasticity and heterotopic ossification, prognosis, rehabilitation strategies, and continuum of care. Teaching rounds will be supplemented by on-site didactics. All WMC-based didactics will be presented on a hybrid platform (remotely and in person) and therefore available for participation from this site.
Teaching Faculty
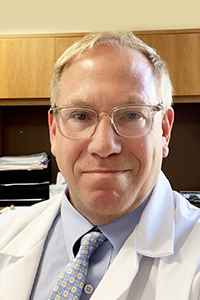
Paul T. Diamond, MD
Residency Program Director
Director and Chief of Service
Professor
Medical School: University of Virginia
Residency (IM): Johns Hopkins Medical Institutions
Residency (PM&R): Sinai Rehabilitation Center / Johns Hopkins

Ruth Alejandro, MD
Site Director: Blythedale Children's Hospital - Pediatric Rehabilitation
Clinical Assistant Professor
Medical School: New York Medical College
Residency: New York Presbyterian – Columbia & Cornell – PM&R

Kathy Aligene, MD
Medical Director, PM&R Outpatient Specialty Practices
Clerkship Co-Director
Clinical Assistant Professor
Medical School: St. George's University
Residency: Icahn School of Medicine at Mount Sinai – PM&R
Fellowship: Icahn School of Medicine at Mount Sinai – Pain Medicine

Mark Bodack, MD
Site Director: MidHudson Regional Hospital
Medical School: The Royal College of Surgeons in Ireland
Residency: New York Hospital – Cornell – PM&R
M. DiMattia, MA, CCC-SLP
Director, Speech Language Pathology
Westchester Medical Center

Carolin Dohle, MD
Section Chief – Inpatient Neurology
Clinical Assistant Professor
Medical School: Ruhr-University, Bochum, Germany
Residency: Yale New Haven Hospital - Neurology
Fellowship: Burke Rehabilitation Hospital - Neurorehabilitation

Rhea Dornbush, PhD
Clinical Neuropsychologist
Professor of Clinical Public Health / Psychiatry and Behavioral Sciences
Graduate School: Queens College, CUNY – Clinical Neuropsychology
Graduate School: City University of New York – Psychology

Negin Gohari, DO
Clinical Assistant Professor
Medical School: New York College of Osteopathic Medicine
Residency: North Shore Long Island Jewish Hospital – PM&R
Stephen Kornfeld, DO
Site Director: James J. Peters VAMC – Spinal Cord Injury
Clinical Assistant Professor
Medical School: Western University of Health Sciences
Residency: Mt. Sinai Medical Center – PM&R

Anusha Lekshminarayanan, MD
Sports Medicine Program at WMC
Clinical Assistant Professor
Medical School: S.B.K.S Medical Institute and Research Centre
Residency: New York Medical College / Metropolitan – PM&R
Fellowship: Montefiore – Sports Medicine

Jin Li, MD, PhD
Electrodiagnosis Service
Chief Neuromuscular Section, WMC
Medical School: Beijing Medical University
Residency: New York Medical College – Neurology
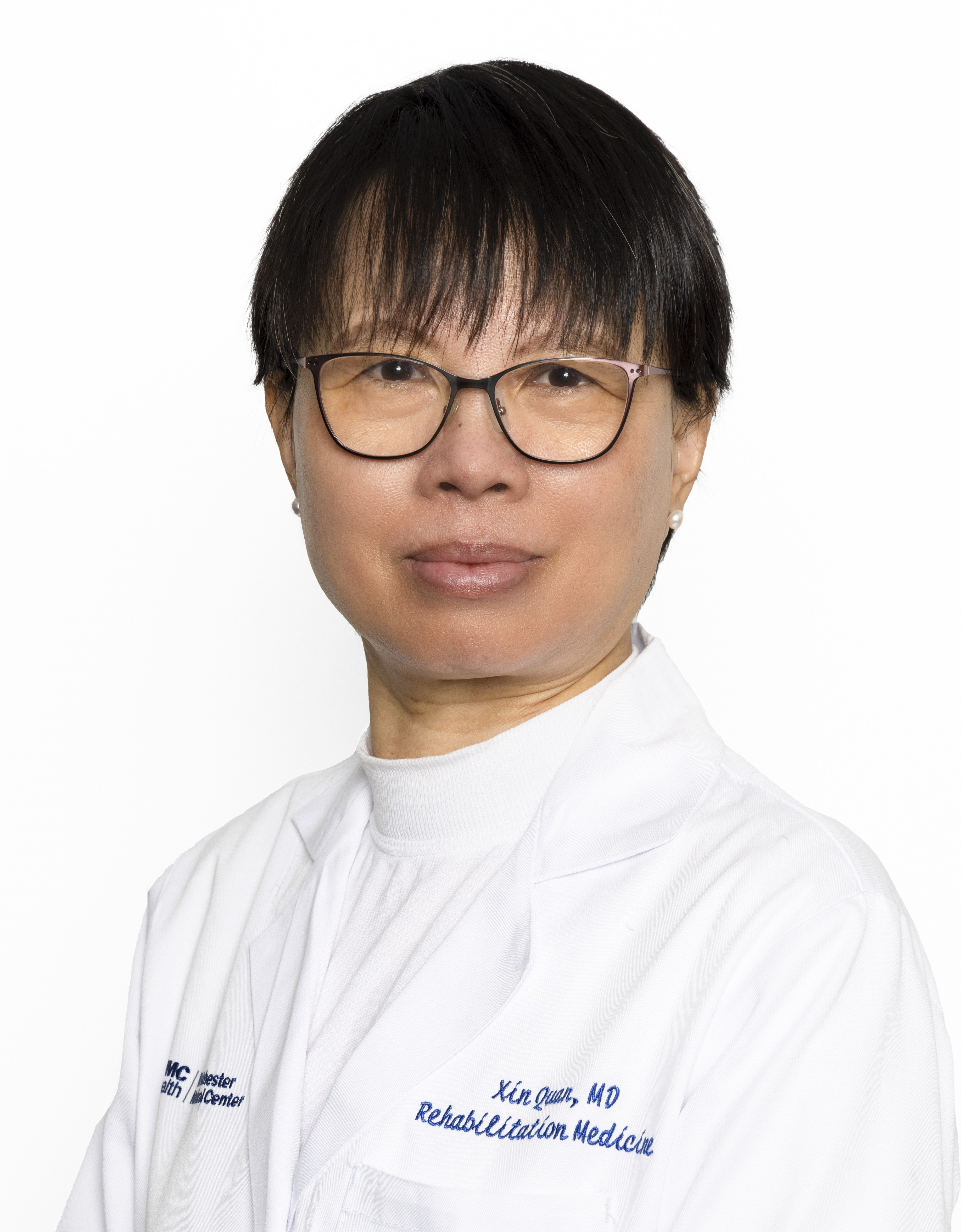
Xin Quan, MD
Clinical Assistant Professor
Medical School: Beijing Medical University
Residency: New York Medical College / Metropolitan – PM&R

Salem Latif, MD
PGY 1 (Fundamental Clinical Skills Year) Supervisor
Medical School: St. George's University
Residency: New York Presbyterian – Brooklyn Methodist Hospital

Sheila Maguire, MSPT
Supervisor, Physical Therapy Services
Westchester Medical Center
J. Kahan McLear, MA, OTRL/L
Supervisor, Occupational Therapy Services
Westchester Medical Center
Jordan Stumph, MD
Associate Medical Director, WMC Inpatient Unit
Clinical Assistant Professor
Medical School: Albert Einstein
Residency: New York Presbyterian – Columbia and Cornell – PM&R

Anila Thomas, MD
Electrodiagnosis Service
Assistant Professor
Medical School: New York University
Residency: Mt. Sinai School of Medicine - Neurology
Fellowship: Mt. Sinai School of Medicine – Clinical Neurophysiology

Xiaofang Wei, MD
Pediatric Physiatrist, Blythedale Children's Hospital
Medical School: Hubei Medical University
Residency: New York Medical College / Metropolitan – PM&R

S. Zolfaghari, MD, CMD
Site Director: The Grove Rehabilitation and Nursing Center
Medical School: Kermanshah University of Medical Sciences
Residency: Mt. Sinai School of Medicine / James J Peters VAMC – IM
Fellowship: Albert Einstein – Geriatric Medicine