Welcome
Welcome to our exciting Neurocritical Care Fellowship Training Program, one of the newest in the United States. The Neurocritical Care Fellowship at Westchester Medical Center, in affiliation with New York Medical College, is currently accredited by the ACGME and the United Council of Neurologic Subspecialties (UCNS).
The Neuroscience Intensive Care Unit at Westchester Medical Center (WMC) in Valhalla, NY, is a 19-bed closed unit equipped with video-EEG and Moberg CNS multimodality monitors in every room. WMC, the flagship of the Westchester Health Network, is the only Level 1 Trauma Center and Comprehensive Stroke Center between New York City and Albany, and draws as the main referral center for 2.8 million people in the Hudson Valley.
Our mission is to create a world renowned Neurocritical Care training program that provides trainees with the knowledge to manage and to study common and rare conditions seen in the Neurocritical Care population. Our goal is to educate and to discover optimal treatments for patients with life threatening nervous system injury. Along the way, trainees will potentially have the opportunity to combine their Neurocritical Care Fellowship training at Westchester Medical Center with additional training in Vascular Neurology (one year) or Neuro-Interventional Surgery (two years). With a dedicated, multidisciplinary core faculty, an advanced Neuroscience Intensive Care Unit, ongoing clinical trials, and the support of the Westchester Medical Center Health Network, this is an exciting time of growth and innovation for our program, which I invite you to explore.

Dr. Stephan A. Mayer
Director of Neurocritical Care
Neurocritical Care Fellowship Program Director
stephan.mayer@WMCHealth.org
914.493.3115
Neurocritical Care Introduction with Stephan Mayer, MD from WMCHealth.
Curriculum
Fellows will gain expertise in the management of critically ill patients. In addition to standard critical care resuscitation techniques such as intubation, mechanical ventilation, volume resuscitation, and vasopressor use, the program emphasizes advanced multimodality monitoring, electroencephalography, and Critical Care Neurophysiology.
Our program serves a large and diverse patient population, and we as faculty will provide individualized training and mentorship that is personalized to meet the interests and background of the fellow. A major point of differentiation is our emphasis on clinical research training and methodology. Development of independent research projects is strongly encouraged, and fellows will benefit from close mentoring and exposure to database management, biostatistics, and study design.
The fellowship is a two-year training program (see below) consisting of 13 four-week block rotations per year, thus providing broad critical care exposure. We also offer a one year training program for applicants with prior training in Neurosurgery or Critical Care who meet ACGME criteria for the accelerated track.
| Neuro-ICU |
9 blocks |
Selective (MICU, TICU, Endovascular Anesthesia/Airway...)
|
5 blocks |
Electives
|
6 blocks |
| Night Float |
4 blocks |
| Vacation |
2 blocks |
Curriculum over two academic years
Fellows will become proficient in ultrasound-guided central venous and arterial catheter placement, lumbar puncture, fiberoptic bronchoscopy, endotracheal intubation, percutaneous thoracostomy, thoracentesis, continuous EEG monitoring, ventriculostomy management, point of care ultrasound, and ventilator management.
In addition to a core Neurocritical Care Journal club, our fellows participate in an organized series of lectures and teaching conferences with Neurology, Neurosurgery, and Pulmonary Critical Care. Upon completion, fellows will be proficient in the management of a wide range of neurological and general critical care conditions and board eligible for the UCNS and ABPN/ABMS Neurocritical Care certification exams.
|
Didactic Schedule
|
Day/Time
|
|
Weekly
|
|
|
Endovascular/Stroke Conference
|
Tuesday
7:30–8:00
|
|
Neurosurgery Chief of Service Rounds
|
Wednesday
8:30–9:30
|
|
Critical Care Fellow Boot Camp Lecture Series
|
Thursday
1:00–2:00
|
|
Neuroradiology Conference
|
Thursday
1:30–2:30
|
|
ICU EEG review
|
Friday
11:30–12:00
|
|
Neurology Grand Rounds
|
Wednesday
1:30–2:30
|
|
Monthly
|
|
|
Critical Care Grand Rounds
|
Tuesday
3:00–4:00
|
|
NSICU and Neurosurgery Quality Improvement Conference
|
Wednesday
8:30–9:30
|
|
Neurosurgery Grand Rounds
|
Wednesday
8:30–9:30
|
|
NSICU Journal Club / Core Lecture Series
|
Tuesday
1:30–2:30
|
|
Neurosurgery / Neurocritical Care Research Updates
|
Wednesday
11:00–11:30
|
|
Point of Care Ultrasound Lecture Series
|
Thursday
4:00–5:00
|
|
Electroencephalography / Neurophysiology Conference
|
Wednesday
12:30–1:30
|
|
Quarterly
|
|
|
Joint Cerebrovascular Conference
|
Wednesday
9:30–10:30
|
|
Annually
|
|
|
Sedation and Intubation Simulation module with Anesthesia
|
|
|
Critical Care Ultrasound Training Course
|
|
Four weeks of vacation time are allotted per year. Salary is commensurate with PGY level. Information on salary and benefits are accessible here.
Our Research
In addition to teaching and providing patient care, the Westchester Medical Center Neurocritical Care faculty are prolific academicians, producing approximately 40 original research papers and multiple specialty medical meeting presentations each year. We equally emphasize the generation of original research projects, as well as participation in national and international clinical trials funded by the National Institutes of Health, as well as industry.
Our goal is to help develop our students, residents, and fellows to become the next generation of academic neurointensivists and clinician-investigators.
Resident Elective Rotations
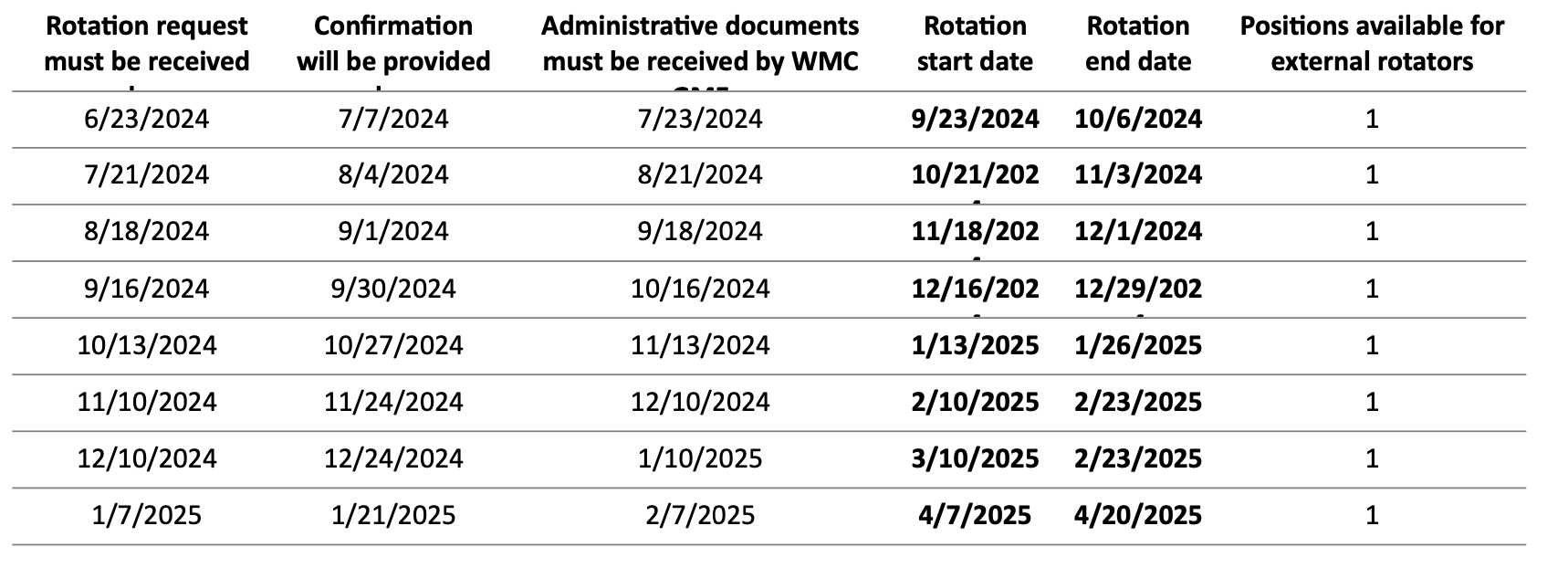
We are happy to host resident rotators from other residency programs that do not offer training in a Neurocritical Care environment, with a preference for those with significant prior neurology exposure and/or those interested in fellowship training in Neurocritical Care. Pre-approved and credentialed in-rotators are privileged to fully participate in patient care as a member of the Neurocritical Care team. In-rotators also receive a formal written evaluation. In-Rotations are contingent upon department and Westchester Medical Center Graduate Medical Education approval. Salary, fringe and malpractice must remain covered by the rotator’s home institution. Note that to maintain a high-quality educational experience for all, rotations are available for a limited number of specific blocks which are 2 weeks in duration.
Interested applicants should send their CV and desired rotation dates / block (see schedule below) to Dr. Andrew Bauerschmidt at andrew.bauerschmidt@WMCHealth.org.
Visiting resident rotator blocks available and application timeline:
Medical Student Rotations
We are pleased to offer a popular one-month neurocritical care medical student elective rotation. Students at New York Medical College as well as other LCME- or AOA-accredited medical schools are eligible to apply. Students at schools other than NYMC must apply via the Visiting Student Application Service (VSAS). Visiting Student Learning Opportunities™ (VSLO®) | Students & Residents. Only one student rotates per month, and selection is first come, first served, thus visiting students are encouraged to express interest for the upcoming academic year. NYMC students will be given preference when there are multiple requests for a given month. Students are expected to actively participate in rounds, and follow up to three patients. There is a subinternship format available for fourth year students which involves graded responsibility, participation in or observation of ICU procedures, one to two nights of long call per week, and weekend attendance. Students will be formally evaluated and will receive feedback on a regular basis. The grading format is Honors, High Pass, Pass, Fail. Students with excellent performance may request a letter of recommendation at the completion of the rotation. For more information, please contact Dr. Fawaz Al-Mufti at Fawaz.Al-Mufti@WMCHealth.org and visit the NYMC visiting student website.
Neurocritical Care Fellows
Recent Alumni
Anish Thomas, MD
Neurocritical Care Fellow Class of 2024
Medical School: American University of Antigua College of Medicine
Residency: Internal Medicine, St John’s Riverside Hospital, Yonkers, NY
Current Fellows

Stuart Brill, DO
Medical School: Kansas City University of Medicine & Biosciences College of Osteopathic Medicine
Residency: Garden City Hospital, Garden City, MI

Mohamed Barania
Medical School: Al-Azhar Faculty of Medicine for Men in Asyut. Cairo, Egypt
Residency: Al-Azhar University, Cairo Egypt
Fellowship: Royal College of Surgeons England. London, England
Neurocritical Care Faculty
Fawaz Al Mufti, MD
Director of Neuroscience Intensive Care Unit
Director of the Neuroendovascular Surgery Fellowship
Director of the Center for Research and Innovation
- Neuroendovascular Surgery
- Neurointensive Care
- Neurological Surgery
Chirag Gandhi, MD
Chair and Professor, Neurological Surgery
Director, Brain and Spine Institute
- Neuroendovascular Surgery
- Open Cerebralvascular Surgery
- Neurological Surgery
Stephan Mayer, MD
Director of Neurocritical Care and Emergency Neurological Services
Neurocritical Care Fellowship Program Director
Professor, Neurology and Neurosurgery
Jon Rosenberg, MD
Assistant Professor of Neurology and Neurosurgery
Associate Program Director Neurocritical Care Fellowship
John Wainwright, MD
Attending Neurosurgeon, Spine Division
Assistant Professor of Neurosurgery and Orthopedic Surgery
Faculty Publications
View a selection of our 90+ peer-reviewed scientific papers published in 2022-2023:
Asif KS,…..Al-Mufti F…..Potter-Vig J. Mechanical thrombectomy global access for stroke (MT-GLASS): a mission thrombectomy (MT-2020 Plus) study. Circulation. 2023 Apr 18;147(16):1208-20.
Dicpinigaitis A…..Mayer SA, Al-Mufti F. Endovascular thrombectomy for pediatric acute ischemic stroke. Stroke. 2022 May;53(5):1530-9.
Kuohn LR…..Mayer SA. Early deterioration, hematoma expansion, and outcomes in deep versus lobar intracerebral hemorrhage: the FAST trial. Stroke. 2022 Aug;53(8):2441-8.
Dicpinigaitis AJ…..Mayer SA, Al-Muft F. Real‐World Outcomes of Endovascular Thrombectomy for Basilar Artery Occlusion: Results of the BArONIS Study. Annals of Neurology. 2023 Mar 10.
Shu L…..Al‐Mufti F. Perioperative Acute Ischemic Stroke in Patients with Atrial Fibrillation. Annals of Neurology. 2023 May 15.
Shapiro SD…..Mayer SA…..Al-Mufti F. Investigating outcomes post–endovascular thrombectomy in acute stroke patients with cancer. Neurology. 2022 Dec 6;99(23):e2583-92.
Bauerschmidt A ….Rosenberg J, Al-Mufti F. Modern Sedation and Analgesia Strategies in Neurocritical Care. Current Neurology and Neuroscience Reports. 2023 Apr;23(4):149-58.
Fortunato M…..Al-Mufti F. Frailty as a Predictor of Outcomes in Subarachnoid Hemorrhage: A Systematic Review and Meta-Analysis. Brain Sciences. 2023 Oct 23;13(10):1498.
Elfil M….. Al-Mufti F…..Gonzalez-Castellon M. Repeated mechanical thrombectomy for recurrent large vessel occlusion: A systematic review and meta-analysis. Interventional Neuroradiology. 2022 Oct 26:15910199221134307.
Dicpinigaitis AJ…..Mayer SA, Al-Mufti F. Endovascular thrombectomy with and without preceding intravenous thrombolysis for treatment of large vessel anterior circulation stroke: A cross-sectional analysis of 50,000 patients. Journal of the Neurological
Sciences. 2022 Mar 15;434:120168.
Henson T…..Al‐Mufti F, Mayer SA. Outcome and prognostication after cardiac arrest. Annals of the New York Academy of Sciences. 2022 Feb;1508(1):23-34
Elfil M, Ghaith HS, Bayoumi A, Elmashad A, Aladawi M, Al-Ani M, Najdawi Z, Mammadli G, Russo B, Toth G, Nour M. Impact of pre-treatment cerebral microbleeds on the outcomes of endovascular thrombectomy: A systematic review and meta-analysis.
Journal of Stroke and Cerebrovascular Diseases. 2023 Oct 1;32(10):107324.
Aboul-Nour H…..Mayer SA. Mechanical Thrombectomy for Acute Ischemic Stroke in Metastatic Cancer Patients: A Nationwide Cross-Sectional Analysis. Journal of Stroke. 2023 Jan 3;25(1):119-25.
Parnia S…..Mayer SA, TS Shirazi. Guidelines and standards for the study of death and recalled experiences of death––a multidisciplinary consensus statement and proposed future directions. Annals of the New York Academy of Sciences. 2022 May;1511(1):5-21.
Kondziella D….. Mayer SA…..Rass V. Incidence and prevalence of coma in the UK and the USA. Brain communications. 2022 Oct 1;4(5):fcac188
Zhong AJ…..Mayer SA….. Al-Mufti F. Transcarotid access for mechanical thrombectomy in acute ischemic stroke: a meta-analysis and systematic review. Journal of Stroke and Cerebrovascular Diseases. 2022 May 1;31(5):106428.
Taccone FS, Donadello K, Mayer SA. Manipulating temperature: devices for targeted temperature management (TTM) in brain injury. Intensive Care Medicine. 2022 Oct;48(10):1409-12.
Bruder N…..Mayer SA. The REACT study: design of a randomized phase 3 trial to assess the efficacy and safety of clazosentan for preventing deterioration due to delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. BMC Neurology. 2022 Dec;22(1):1-5.
Reznik ME…..Mayer SA…..Jones RN. A pilot study of the fluctuating mental status evaluation: a novel delirium screening tool for neurocritical care patients. Neurocritical Care. 2023 Apr;38(2):388-94.
Vazquez S…..Mayer SA…..Bauerschmidt A…..Al-Mufti F. Incidence and Risk Factors for Acute Transient Contrast‐Induced Neurologic Deficit: A Systematic Review With Meta‐Analysis. Stroke: Vascular and Interventional Neurology. 2022 Jan;2(1):e000142.
Clare K…..Rosenberg J, Bauerschmidt A…...Mayer SA…..Al-Muft F. Safety and efficacy of a novel robotic transcranial doppler system in subarachnoid hemorrhage. Scientific Reports. 2022 Feb 10;12(1):2266.
Additional publications have appeared in various journals including Stroke, Critical Care Medicine, Neurology, PNAS, Epilepsia, Anesthesiology, Journal of Cerebral Blood Flow & Metabolism, American Society of Neuroimaging, Resuscitation, Journal of Neurosurgery, Annals of Biomedical Engineering, Neurocritical Care, and others.
How to Apply
To apply to the Neurocritical Care clinical fellowship program at Westchester Medical Center, in affiliation with New York Medical College, please visit the SF Match website. The site contains important deadline dates to review before applying. Interviews are scheduled in the winter and spring 18 months in advance of the start of the fellowship. Interviews will be conducted virtually.
Requirements and Eligibility
The applicant must be enrolled in or a graduate of a residency program in neurology, neurological surgery, internal medicine, anesthesiology, surgery, child neurology, or emergency medicine that is accredited by the ACGME, ACGME-I, AOA, RCPSC or CanERA, or have completed a minimum of four years of post-graduate clinical training in neurological surgery and be currently enrolled in an ACGME- or CanERA-accredited neurological surgery residency program. Information about applying for a New York State Medical License can be obtained by calling (518) 474-3817. Graduates of international medical schools are eligible to apply. Westchester Medical Center only sponsors J-1 visas (and H-1B visas in certain circumstances) through ECFMG.
Timetable
See SF Match website for our Neurocritical Care Fellowship application timeline
Contact Us
Christine Loscri
Residency & Fellowship Coordinator
Department of Neurosurgery
Christine.Loscri@wmchealth.org
914.493.8795
Stephanie Litt
Administrative Assistant
Department of Neurosurgery
Stephanie.Litt@wmchealth.org
914.493.5216
Dr. Stephan A. Mayer
Neurocritical Care Fellowship Program Director
Director of Neurocritical Care
Stephan.Mayer@WMCHealth.org
914.493.3115
Dr. Jon Rosenberg
Neurocritical Care Associate Fellowship Program Director
Jon.Rosenberg@wmchealth.org